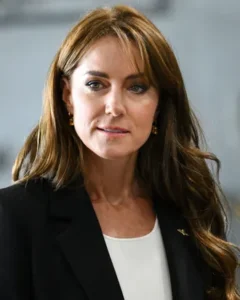
When Kate Middleton announced Friday that she had been diagnosed with cancer and had begun treatment, the development was shocking — even though it had been clear for weeks that something was very wrong. But it also rang familiar.
Judging by our social-media feeds, it certainly feels like more young people are receiving cancer diagnoses. Kate is 42. Earlier this month, actress Olivia Munn, who is 43, announced in an Instagram post that she was diagnosed with breast cancer last year and has undergone four surgeries, including a double mastectomy, in the past ten months. Also this month, Jessica Pettway, a beauty influencer whose hair tutorials built her an early YouTube following, died of cervical cancer at 36. These recent cases call to mind those of Chadwick Boseman, the Black Panther star who died in 2020 from colon cancer, at age 43, and Virgil Abloh, the iconic fashion designer who died in 2021 from cardiac angiosarcoma, a rare heart cancer, at age 41.
Though of course it affects children and young adults, cancer has traditionally been a condition primarily associated with older people; most cancers in the U.S. are found in people ages 65 and up. New research, however, suggests that calculus might be shifting a bit and that cancer rates really are rising among younger people — women in particular.
One recent study looking at 29 cancers in 204 countries found that there’s been a 79 percent increase in early-onset cancers — diagnoses in those under 50 — since 1990. Another recent study in JAMA Network Open found that, while cancer rates for older adults have dropped, during the period from 2010 to 2019, U.S. diagnoses rose nearly 20 percent just among people in their 30s. This spike has been driven in part by increased rates in women: Early-onset diagnoses of all cancers dropped nearly 5 percent in men over the decade, but rose more than 4 percent in women, primarily due to uterine and breast cancers. But researchers are seeing increases in many kinds of cancer. Diagnoses of gastrointestinal cancers — affecting organs including the colon, appendix, and bile duct — increased most quickly, rising about 15 percent.
The research also found that — despite continued decreases in cancer fatalities overall — more young people are dying from cancer. In 2019, there were more than one million deaths globally from early-onset cancer, up nearly 28 percent from 1990. Other research shows that uterine cancer is killing more women across age groups and striking more under 50. The trends are distressing and hard to make sense of, especially for young women patients whose complaints have historically been dismissed.
Doctors don’t know why cancer is affecting more young people. The increase in cases is probably due to a variety of factors, including elements of our modern-day diets, lifestyles, and exposure to pollutants, according to Dr. Andrea Cercek, gastrointestinal oncologist and co-director of the Center for Young Onset Colorectal and Gastrointestinal Cancers at Memorial Sloan Kettering Cancer Center in New York. In the case of the gastrointestinal cancers she treats, that might be processed foods, microplastics, medications like antibiotics, or some combination of the above.
“It’s something that everyone’s exposed to, but there’s a population of young adults that are at risk for that exposure to lead to cancer,” she told me. “The key is to identify who that group is.”
To minimize the risk of developing cancer, physicians including Dr. Cercek urge a heart-healthy diet, regular exercise, weight management, and routine medical care, including the recommended screenings for your age group (if you’re at average risk), such as Pap smears to screen for cervical cancer beginning at age 21 and mammograms for breast cancer starting at 40. In 2018, the American Cancer Society began recommending people get colonoscopies to screen for colorectal cancer starting at 45, rather than 50. (If you’re at higher risk, those guidelines might look different.)
Given the upswing in early-onset cases, though, should screenings start even earlier for people at average risk? Dr. Cercek wasn’t so sure. Though the rates of younger people diagnosed with breast, uterine, colorectal, and other cancers are rising, the overall numbers remain low, she said, and changing the guidelines to include new, large groups of individuals could cause logistical and financial issues, especially since, for many cancers like those of the pancreas or stomach, reliable screening tools don’t yet exist. For colon cancer in particular, in addition to colonoscopies, she said some blood tests under development show promise, as do stool-sample kits like Cologuard.
Dr. Cercek emphasized the importance of paying attention to symptoms — which could look like any number of persistent issues — and seeking medical care. Gastrointestinal symptoms to watch out for include unexplained weight loss, changes in appetite or bowel habits, or rectal bleeding.
Meanwhile, we are just beginning to grapple with the ramifications of this generational moment in our understanding of this disease and its impact on both public and personal health. When younger people get cancer, there are choices to be made about fertility and long-term financial consequences and particular social needs to consider.
People in their 40s, like Kate Middleton, still make up the bulk of early-onset diagnoses and deaths — a pattern that’s expected to continue for now. It’s worth remembering that we’re getting better at treating nearly all types of cancers, and survival rates are improving. The challenge now is bringing those tools to bear on this rapidly evolving problem.